The ABCDE assessment
Learn the basics of the most important examination!
Every unwell patient you’ll be asked to review needs to be examined using the ABCDE assessment!
Here’s a summary on what it entails ⬇️
A - Airway
Start by speaking to the patient. If they’re able to speak, their airway is patent. If they’re unconscious, their GCS is low, or if they’re making snoring sounds (barring the sleeping patient of course 🙃 in that case just wake them up!), they will need adjuncts.
Airway adjuncts include the Oropharyngeal Airway (OPA) and the Nasopharyngeal Airway (NPA).
OPA is the first step and you need to measure the appropriate size. It should span the length from the incisors to the angle of the mandible. Insert it facing upwards and then rotate midway. If your patient is tolerating it, move to B.
If your patient is not tolerating it (indicated by gagging) then you can use the Nasopharyngeal Airway, which comes in two sizes. The size is selected based on the size of the patient’s nostril. Lubricate it and insert it parallel to the palate (do NOT insert it facing towards the brain 🧠). If it’s doing the job, move to B.
If your patient’s airway is still not maintained, ESCALATE and involve ITU/anaesthesia teams for intubation (depending on DNACPR status).
Video links for OPA and NPA insertion techniques are at the bottom of the page under ‘Further Learning’.
B - Breathing
Note patient’s saturations and Respiratory rate and start them on 15L high flow oxygen (this can always be titrated to saturation later). If the respiratory rate is very low, mechanically ventilate using bag valve mask. You can ask for help and get someone to do that for you while you continue with the rest of your examination.
Get an ABG if the saturation is low.
Request a chest X-Ray
Do a quick chest examination with inspection, chest expansion, trachea position checking whether it’s central or deviated, percussion and auscultation. If you’re happy with breathing, move on to C.
C - Circulation
Note the patient’s Blood Pressure and Pulse. Check their capillary refill time (press on the nail/fingertip of the patient and count to 5, count the number of seconds it takes to come back) and check whether peripheries are warm or cold (if peripheries are cold, do a central capillary refill on the chest).
Make sure you have IV access - insert a cannula, and get bloods and a VBG at the same time, if indicated, take blood cultures and group and save samples.
Get a 12 lead ECG.
When happy with C, move to D
D - Disability
Check the patient’s response using ACVPU (Alert, Confused, Verbal, Pain, Unresponsive) This is an easier alternative to assessing GCS.
Check their pupils
Also check the patient’s blood sugar. If D is good, move to E
E - Exposure
Note Patient’s temperature
Do relevant examination - for example abdominal examination, looking for signs of bleeding, looking at Calves for DVT etc.
Bonus tips
Once you’ve done your A to E assessment, depending on findings, make your management plan and carry that out. Then escalate to your senior (unless of course you’re struggling then involve them early)
Do not move to the next step until the one you’re on is stable. So you cannot move to C until B is stabilised and you can’t get to B until A is sorted.
Tailor E according to your clinical suspicion. For example if a patient who had surgery a few weeks ago presents with sudden shortness of breath with oxygen requirement and you are suspecting Pulmonary Embolism, then check calves for signs of DVT.
It helps to clarify the DNACPR status early to plan your next steps and whether the patient will be requiring CPR and that way you can put out a peri arrest call if your findings show a severely decompensated patient who might go into cardiac arrest or will need ITU admission.
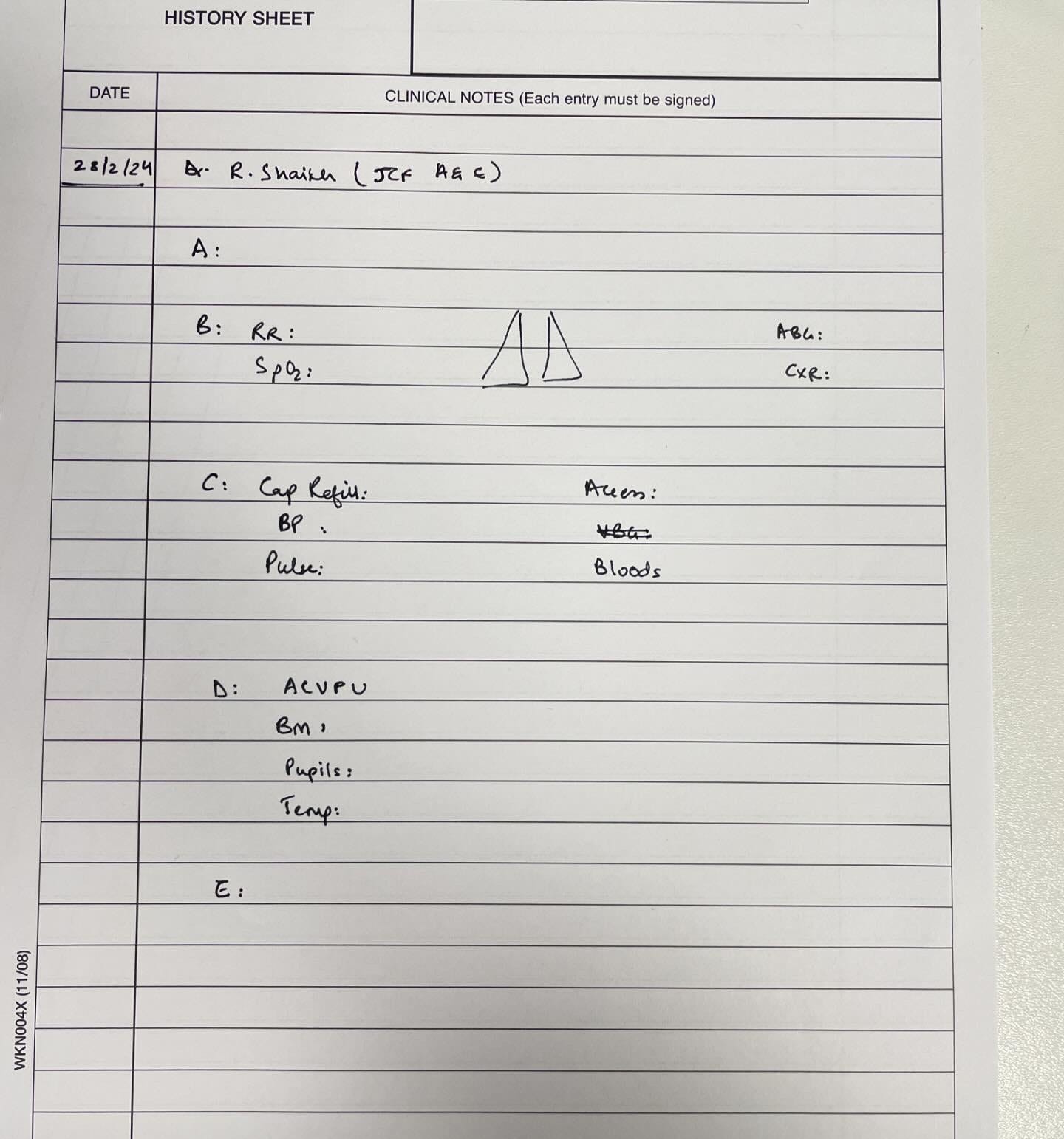
Here’s how to document your A to E assessment. I have missed writing ECG and wrote Temperature in D 🙈 but I did write it all properly later on
Further learning:
Video demonstrating an A to E assessment.
Video for OPA insertion
Video for NPA insertion
Comment any questions you have below!


Suppose we are seeing a fracture case (interview point of view), should we do local examination in exposure ? And take relevant history after Abcde ?
Very well defined 👍